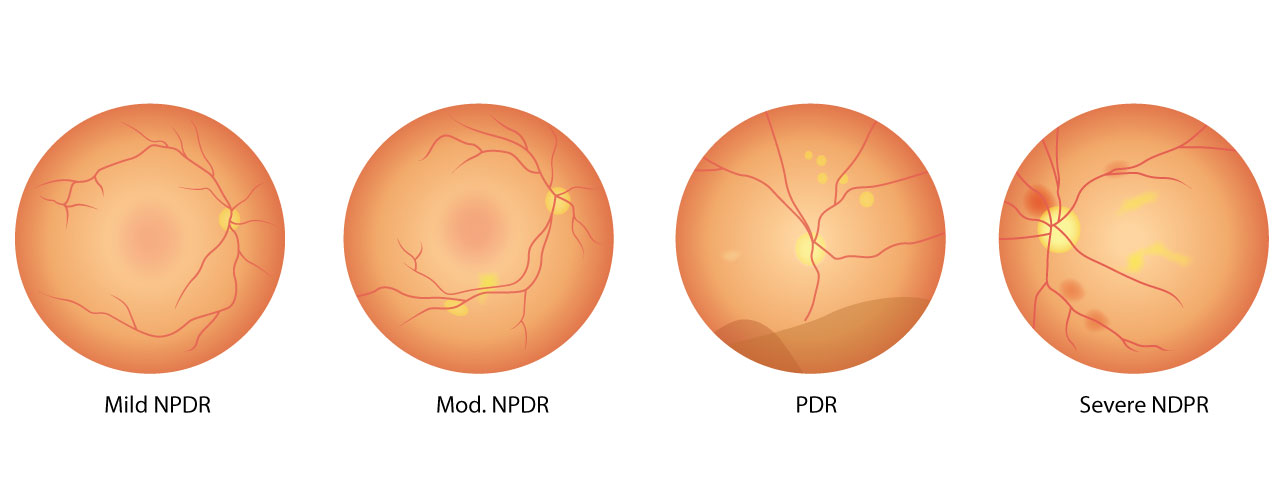
The 4 Stages of Diabetic Retinopathy
Diabetic retinopathy is an eye disease that develops when high blood sugar damages the tiny fragile blood vessels in the retina of people living with diabetes.
This progressive eye disease may lead to blurred vision or even irreversible vision loss. Regular eye exams are important, because, by the time noticeable symptoms appear, vision loss may have occurred. The sooner your eye doctor can diagnose diabetic retinopathy, the sooner you can take steps to slow its progression.
What Are the Stages of Diabetic Retinopathy?
There are two types of diabetic retinopathy, which progresses in four stages.
The two types of diabetic retinopathy are nonproliferative and proliferative. Nonproliferative refers to the early stages of the disease, while proliferative is an advanced form of the disease.
Stage 1: Mild nonproliferative diabetic retinopathy
This is the earliest stage of diabetic retinopathy, characterized by tiny swellings/bulges in the blood vessels of the retina. These areas of swelling are known as microaneurysms.
These microaneurysms can cause small amounts of fluid to leak into the retina, triggering swelling of the macula – the back of the retina. Despite this, there are usually no clear symptoms indicating there is a problem.
Stage 2: Moderate nonproliferative diabetic retinopathy
At this stage, the tiny blood vessels further swell up, blocking blood flow to the retina and preventing proper nourishment. This stage will only cause noticeable signs if there is a build-up of blood and other fluids in the macula, causing vision to become blurry.
Stage 3: Severe nonproliferative diabetic retinopathy
During this stage, a larger section of blood vessels in the retina becomes blocked, causing a significant decrease in blood flow to this area. The lack of blood triggers a signal to the body to start growing new blood vessels in the retina.
These new blood vessels are extremely thin and fragile and cause retinal swelling, resulting in noticeably blurry vision, dark spots and even patches of vision loss. If these vessels leak into the macula, sudden and permanent vision loss may occur. At this stage, there is a high chance of irreversible vision loss.
Stage 4: Proliferative diabetic retinopathy
At this advanced stage of the disease, new blood vessels continue to grow in the retina. These blood vessels, which are thin and weak and prone to bleeding, cause scar tissue to form inside the eye. This scar tissue can pull the retina away from the back of your eye, causing retinal detachment. A detached retina typically results in blurriness, reduced field of vision, and even permanent blindness.
What Are Common Symptoms of Diabetic Retinopathy?
During its first two stages, diabetic retinopathy doesn’t usually cause obvious symptoms, so it’s possible to have it and not even know it.
Unfortunately, many people don’t have symptoms until the disease progresses to the proliferative diabetic retinopathy stage.
However, an eye examination by your [eye doctor] can detect diabetic retinopathy in its earlier stages, before symptoms become noticeable and damage has become irreversible.
Symptoms of proliferative diabetic (stage 4) retinopathy include:
- Blurry vision
- Change in colors
- Decrease in field of vision
- Distorted vision
- Increase of eye floaters
- Loss of vision
- Poor night vision
How to Treat Diabetic Retinopathy
While diabetic retinopathy may lead to irreversible vision loss, successfully managing your blood sugar levels can help prevent loss of vision. This includes watching your diet, increasing physical activity, and taking diabetes medication as directed.
Other treatments depend on the stage or extent of the disease. If caught very early — before damage to the retina occurs — blood sugar management might be the only treatment necessary.
If you’re in a nonproliferative stage but experience some eye damage, treatment options might include:
- Eye injections – A steroid injection in the eye to stop inflammation and prevent new blood vessels from forming. Anti-VEGF injections may also be recommended, which can reduce swelling in the macula and improve vision.
- Laser surgery – Laser surgery called photocoagulation reduces swelling in the retina and removes abnormal blood vessels.
- Vitrectomy – If you are in the later stages of diabetic retinopathy, you might need a vitrectomy. This eye surgery treats problems with the retina and vitreous, a jelly-like substance in the middle of the eye. The surgery can remove blood or fluid, scar tissue, and some of the vitreous gel so light rays can focus properly on the retina. Retinal detachments can be corrected at the same time.
Diabetic retinopathy is a potentially serious eye disease that can result in permanent distorted vision or vision loss. Preserve your vision by contacting North Park Vision Center to schedule your comprehensive eye exam today.
Our practice serves patients from Westminster, Broomfield, Thornton, and the Front Range, Colorado and surrounding communities.








